
Skin & Wound
Lesson by Siobhan Bell · 4 years ago ·
Content Blocks
You are working in the emergency department (ED) of a community hospital when the ambulance arrives with Annie, a 28-year-old woman who was involved in a house fire. She was sleeping when the fire started. She managed to make her way out of the house through thick smoke. The EMS Advanced Paramedic crew started 100% humidified oxygen at 15 L/min per non-rebreather mask and started a 16-gauge IV with lactated Ringer’s solution. On arrival in the ED, her vital signs are 100/66, 125, 34, SpO2 93%. She is alert and oriented x 4 and appears anxious and in pain.
Nursing Process - Assessment
Your first step is to obtain a report from the EMS Crew and begin your initial emergency assessment.
INITIAL EMERGENCY ASSESSMENT
- Obtain the history of the injury and confirm all prehospital interventions.
- Follow ABC (Airway, Breathing, Circulation) to ensure patient remains alive in the immediacy.
- Your first action is to evaluate patency of her airway and continue 100% humidified oxygen therapy at 15 L through a non-rebreather mask.
- Have equipment readily available for endotracheal intubation or tracheostomy.
- Start pulse oximetry and continuous ECG monitoring.
- Insert a second large-bore (18 gauge or larger) IV line and begin fluid replacement.
- Perform cardiovascular and peripheral vascular and neurologic assessments.
- Obtain baseline CBC, CMP, ABGs, carboxyhemoglobin levels and weight.
- Give analgesia.
- Elevate burned limbs above the heart.
- Remove non-adherent clothing
- Assess the extent and nature of burns
- Cover burned areas with dry dressings or clean sheet
- Insert an indwelling catheter and nasogastric tube as ordered by the emergency room NP who has joined you during your initial assessment.
- Offer psychological support to Alma and her family.
YOU ARE CONCERNED ABOUT SMOKE INHALATION AND PERFORM A SECONDARY ASSESSMENT AFTER ENSURING YOUR PATIENT IS STABLE
- Assess for burns to the face and neck; singed nasal or facial hair; and cherry-red skin color.
- Cough with or without copious sputum that may or may not be black, gray, carbonaceous, or bloody; smoky breath.
- Inspect the oropharynx and vocal cords for redness, ulcerations, swelling, and blisters.
- Observe Alma for increasing restlessness, dyspnea, difficulty swallowing, increasing hoarseness, stridor, wheezing, and nasal flaring.
- Monitor VS for tachycardia, dysrhythmias, a decrease in oxygen saturation, and rapid, shallow respirations.
- Monitor ABGs and carboxyhemoglobin levels.
- Monitor for neurological changes associated with hypoxia such as restlessness, anxiety, altered mental status, confusion, decreased level of consciousness.
As you perform your initial assessment, you note burns on Alma's right anterior leg, left anterior and posterior leg, and anterior torso. You know you will need to document this using the rule of nines - calculating the extent of Alma's burn injury.
Continued Assessment...
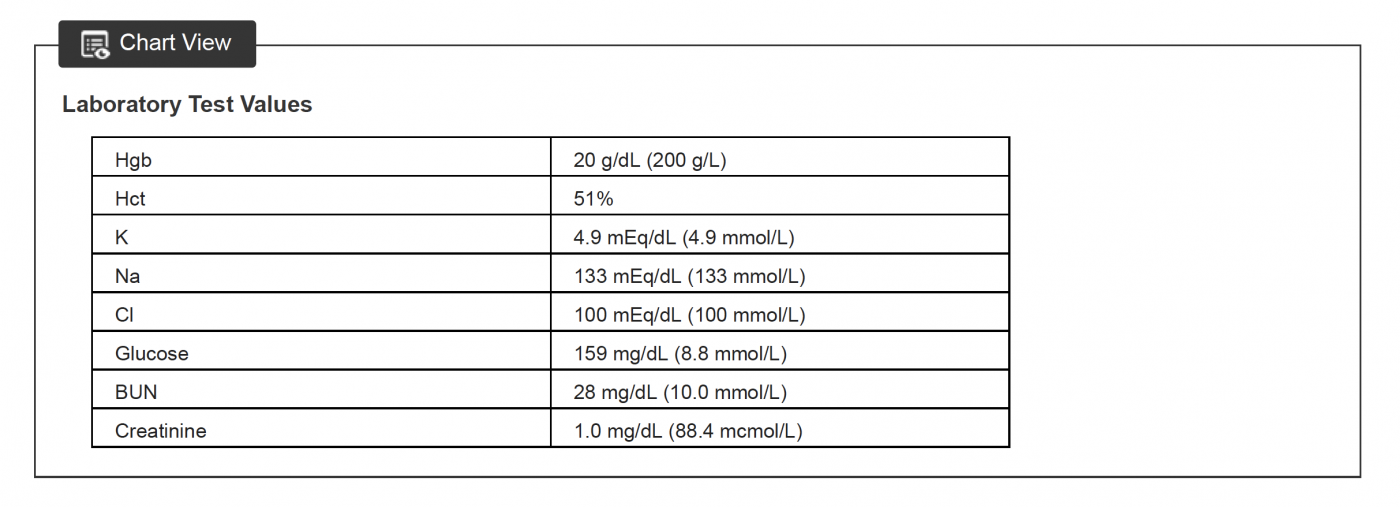
During the initial period of a burn injury, the Hgb and Hct levels increase to above normal because of hemoconcentration from the large fluid shifts and resulting vascular dehydration. Hct levels of 50% to 55% are expected during the first 24 hours after injury, which will return to normal by 36 hours after injury. Na and Cl levels are low because of fluid loss associated with the burn injury and sodium retention in the interstitial spaces. BUN is slightly elevated because of fluid loss. Hyperglycemia occurs during the acute phase because of lipolysis, gluconeogenesis, glycogenolysis, and relative insulin insensitivity.
Nursing Process - Diagnosis/Priority Needs of the Client
When we are looking at "Nursing Diagnosis" what we are really looking for is......
What do I need to DO to help my patient...and within that list of things to do which ones should I do FIRST.
Looking at Alma's case: when you look at all of your assessment data what are your priority actions?
- Maintain Patent Airway
- Restore fluid and electrolyte status (Fluid Resuscitation)
- Pain Control
- Provide Emotional Support to client and clients support system
- Wound and Skin Integrity
- Infection Prevention
Out of those 5 priorities, you will need to continuously assess which one to do first, second, third...and then when to repeat.
For example: If the patient's airway suddenly becomes unstable, you would not continue with wound care while your patient stops breathing.
Nursing Process - Interventions
Note: Every intervention comes from a best practice. Best practice comes from evidence....evidence is derived from research! So this is where you need to have evidence to support your choice of intervention. Interventions also have to be evaluated as to whether you can INITIATE the intervention without an order from the NP/MD or if there is a standing order, or if you need to seek an order before intervening.
Interventions always need to be SMART!!
Remember- They need to be Specific to your intervention, you need to be able to Measure them either quantitatively or qualitatively, they need to be Achievable meaning it is something that you have the resources for and that your client could do (you can't say you will teach a snail to fly...they don't have wings), Relevant meaning it is directly related to your priority need/diagnosis and Timely- This one is VERY important - If your intervention is for an emergent need your timeline needs to reflect that urgency (example: acute pain - you should not be waiting more than 15-20 mins to re-evaluate the effectiveness of pain control when given through IV - 30 min-45 mins for PO pain meds)!
Looking at our priorities above:
1. Patent Airway - The intervention for nurses is to maintain observation and continued assessment of the patient's respiratory status (How?). Do we need an order? Where could you find this as your best practice?
2. Restore fluid and electrolyte status (Fluid Resuscitation) - This intervention requires nurses to administer fluids to replace the loss as well as encourage fluid to navigate back into the cell from outside the cell. What kind of fluid would that be? Do you need an order to administer fluids? Why? Where could you find the evidence of fluid resuscitation and what kind of fluid needed to support your conversation with a NP/MD?
3. Pain Control - This intervention requires nurses to administer either or both pharmacological intervention and/or complimentary therapies. Thinking about this...what is Alma's pain like? How do you know? What would you offer for pain control? why? Do you need an order? Where could you find this evidence to support the best practice?
4. Provide Emotional Support to client and clients support system - What does this intervention look like? What can you offer the client or their support to help them? Do you need an order? Where is the evidence for this intervention?
5. Wound and Skin Integrity - What did the Rule of 9's tell you about her wounds? What do we do for new burns? Do you need an order? Where is the evidence to support this?
6. Infection Prevention - Open wounds and fresh burns - what about a burn makes it specifically more challenging to handle than a regular surgical wound or abrasion? What can we do to help? Standard interventions such as: Place her in a private room and initiate protective isolation procedures. Use aseptic technique with sterile gloves during dressing changes. All supplies necessary for patient should remain in her room. No one with an actual or potential infection should care for or visit her. Provide family education about infection precautions. Administer antibiotics and antipyretics as prescribed. Change bed linens daily and whenever soiled. She would receive a tetanus toxoid because of the chance of anaerobic burn wound contamination. HOW do we know this is best practice? Do we need an order for any of these? Where can we find the evidence to support this?
Nursing Process - Evaluation
Evaluations always need to re-evaluate your SMART interventions using the criteria you established
Remember- They need to be Specific to your intervention, you need to be able to Measure them either quantitatively or qualitatively, they need to be Achievable meaning it is something that you have the resources for and that your client could do (you can't say you will teach a snail to fly...they don't have wings), Relevant meaning it is directly related to your priority need/diagnosis and Timely- This one is VERY important - If your intervention is for an emergent need your timeline needs to reflect that urgency (example: acute pain - you should not be waiting more than 15-20 mins to re-evaluate the effectiveness of pain control when given through IV - 30 min-45 mins for PO pain meds)!
1. Patent Airway - The intervention for nurses is to maintain observation and continued assessment of the patient's respiratory status
- EVALUATION:
2. Restore fluid and electrolyte status (Fluid Resuscitation) - This intervention requires nurses to administer fluids to replace the loss as well as encourage fluid to navigate back into the cell from outside the cell. What kind of fluid would that be? Do you need an order to administer fluids? Why? Where could you find the evidence of fluid resuscitation and what kind of fluid needed to support your conversation with a NP/MD?
3. Pain Control - This intervention requires nurses to administer either or both pharmacological intervention and/or complimentary therapies. Thinking about this...what is Alma's pain like? How do you know? What would you offer for pain control? why? Do you need an order? Where could you find this evidence to support the best practice?
4. Provide Emotional Support to client and clients support system - What does this intervention look like? What can you offer the client or their support to help them? Do you need an order? Where is the evidence for this intervention?
5. Wound and Skin Integrity - What did the Rule of 9's tell you about her wounds? What do we do for new burns? Do you need an order? Where is the evidence to support this?
6. Infection Prevention - Open wounds and fresh burns - what about a burn makes it specifically more challenging to handle than a regular surgical wound or abrasion? What can we do to help? Standard interventions such as: Place her in a private room and initiate protective isolation procedures. Use aseptic technique with sterile gloves during dressing changes. All supplies necessary for patient should remain in her room. No one with an actual or potential infection should care for or visit her. Provide family education about infection precautions. Administer antibiotics and antipyretics as prescribed. Change bed linens daily and whenever soiled. She would receive a tetanus toxoid because of the chance of anaerobic burn wound contamination. HOW do we know this is best practice? Do we need an order for any of these? Where can we find the evidence to support this?
Case Study Outcome
Four days after her injury, Alma is discharged from your medical unit and is admited to the rehabilitation floor where she begins a formal rehabilitation program and is able to maintain full range of motion and tissue mobility. Her recovery is prolonged by two wound infections, and she does experience some scarring.
One year later she is still struggling with adapting to her new body image, but she is finding encouragement from family, friends, and her support group.
Now that you have worked through one priority goal and evaluation/outcome. Go back through the case scenario and identify another priority that you can address and use the below care plan builder to build your own!
Build a Care Plan
Collaborators
License
Skin & Wound by Siobhan Bell is licensed under a Creative Commons Attribution License (CC BY), except where otherwise noted.


Comments
Be the first to comment!