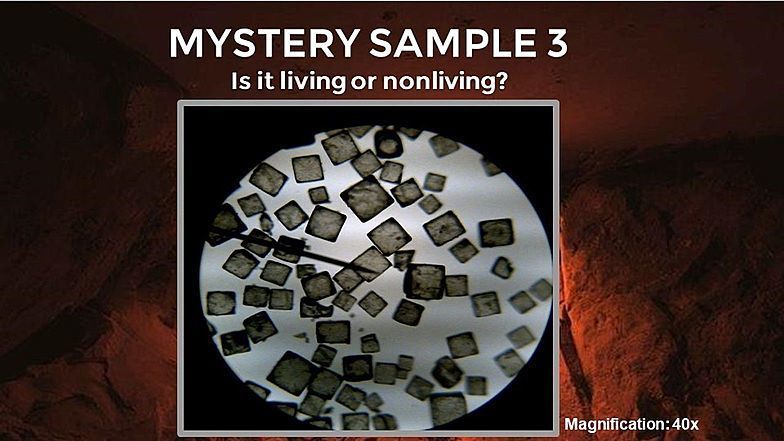
IS IT LIVING!!!!!!
- Read more about IS IT LIVING!!!!!!
- 1 comment
- Log in or register to post comments
- 65 views
life without cells would be helpless we would be weak and the government would have to build more hospitalsImagine a world where we didn't have the amazing power of cells to keep us going. It's hard even to fathom, but our bodies would be helpless and we would be weak. Just think about all the incredible things we can accomplish because of our cells - we can run, jump, dance, and explore the world around us. Let's never take for granted the incredible gift of life that our cells give us, and let's use that gift to inspire others and positively impact the world. Remember, you have the power to do amazing things - all thanks to the incredible cells that make up your body! and well no one would have the energy to give commands and move around to build the hospital
Login or register to join the discussion.
Discussions
Login or register to share your adaptations.
List of adaptions
Be the first to add your adaptation here!
Login or register to engage in the review and feedback process.
Reviews and Feedback
Be the first to review!














Comments
hope you enjoy this short article